Robotic-assisted laparoscopic partial nephrectomy
What is a partial nephrectomy?
A partial nephrectomy is an operation to remove part of your kidney that has disease or tumour within it. This enables you to have disease removed but also to preserve your kidney and its function. The surrounding fatty tissue, lymph nodes, adrenal gland and upper end of your ureter (tube carrying urine from the kidneys to the bladder) are not removed as they are in a radical (total) nephrectomy.
A partial nephrectomy is usually performed when tumours are less than 4cm wide however recent recommendations have extended it to upto 7cm and beyond if more than 30% of the renal parenchyma could be preserved.
What is an open partial nephrectomy?
An open partial nephrectomy is the traditional operation for removing a particular part of the kidney. The surgeon makes an incision (cut) about 15-20cm (6-8 inches) long, allowing enough room to remove the disease from a kidney.
An open partial nephrectomy is required if it is not technically possible or considered too difficult to remove part of the kidney using keyhole (laparoscopic) techniques
What is laparoscopic surgery?
Laparoscopic surgery is keyhole surgery that is performed without having to make a large incision. Instead, surgery is carried out using small keyhole instruments that are inserted into
the abdomen (tummy) via small incisions. The abdomen is filled with carbon dioxide gas so that the internal organs can be seen. However rigid instrumentation of laparoscopy prevents proper dissection and suturing during the surgery thus compromising results and higher complications.
What is robotic-assisted surgery?
This is advance laparoscopic surgery using robotic assistance through the small keyhole incisions. The keyhole instruments and a camera allowing the surgeon to see inside of your abdomen are attached to the robotic arms.
Dr. Gandhi, in Ruby hall clinic is the only surgeon in Pune trained to offer robotic-assisted surgery for urological procedures especially robotic partial nephrectomy.
What is a robotic-assisted laparoscopic partial nephrectomy?
A robotic-assisted laparoscopic partial nephrectomy is keyhole surgery to remove a diseased part from a kidney using the da Vinci® Si robotic system.
The da Vinci® robot provides high-definition imaging and a three-dimensional (3D) view of your abdomen for the surgeon. Ruby Hall Clinic hospital has the latest da Vinci® Si robot. Dr. Gandhi is the most experienced robotic surgeon in Pune and in India. The da Vinci® Si system allows the surgeon higher levels of precision during the tumour removal and reconstruction (rebuilding) of the kidney during the procedure than standard laparoscopy.
Why should I have a robotic-assisted laparoscopic partial nephrectomy?
Your doctor will have already discussed with you why he/she recommends you should have this procedure. The benefits of keyhole surgery, compared with open surgery, include:
- Smaller scars and less muscle damage
- Shorter hospital stay (usually two to three days)
- Less pain after the operation
- Quicker full recovery and earlier return to work.
Robotic-assisted surgery also offers quicker and more precise suturing (stitching) compared with standard keyhole surgery.
What are the risks?
As with any surgery, there are some risks associated with this procedure. There are no additional risks for robotic surgery over non-robotic surgery. Some of the more common risks include:
- Bleeding requiring blood transfusion (occurs in fewer than two out of every 100 procedures). Occasionally a bleeding blood vessel can be blocked in the x-ray department using angiography (blood vessel imaging).
- Damage to structures around the kidney, including the spleen, colon, liver, pancreas or bowel (one in 100).
- Urinary leak around the kidney or bleeding into the ureter tube (three to five in 100). This may require a prolonged hospital stay, insertion of a ureteric stent (internal drainage tube into the ureter) or re-insertion of a drainage tube through the skin.
- The need to convert to open surgery due to robot failure, bleeding or other complications.
- The need to perform a total (radical) nephrectomy if partial nephrectomy is not technically possible.
- Complications associated with general anesthetics, such as irregular heartbeat, chest infection, or blood clots in the legs (deep vein thrombosis or DVT) or lungs (pulmonary embolism).
- We may find that the tumour removed is not cancerous and is a relatively harmless benign growth (one in 10 to 20).
- Late complications, for example hernia at the wound sites, scaring or cancer recurrence.
- The risk of dying from laparoscopic urologic surgery is extremely low (about three to eight in 10,000).
Your doctor will discuss these risk factors with you in detail. If you have any questions, concerns or need further information, please feel free to ask them.
How can I prepare for my procedure?
You will attend a pre-assessment clinic before your surgery. It is very important that you come to this appointment, as this is when we will assess your suitability and fitness for surgery and anesthetic. We will carry out a number of tests to make sure that your heart, lungs and kidneys are working properly. You may have a chest x-ray, ECG or electrocardiogram (which records
the electrical activity of your heart) and some blood tests. Your doctor will explain any further tests you may need.
If you do not attend this appointment, we may have to cancel your surgery.
Smoking
If you smoke, you may be asked to stop, as smoking increases the risk of developing a chest infection, or a blood clot in the leg (deep vein thrombosis or DVT) or lung (pulmonary embolism). Smoking can also delay wound healing because it reduces the amount of oxygen that reaches the tissues in your body.
Medicines
If you are taking any medication, these may need to be temporarily stopped or adjusted around the time of your surgery, you will be given information on how to do this at your pre-assessment appointment. Do not make any changes to your usual medicines and continue to take them unless you have been advised to do so. Please remember to bring them into the hospital with you.
If you are taking any medicines that thin your blood, such as antiplatelet medicines (for example aspirin or clopidogrel) or anticoagulant medicines (for examples warfarin or rivaroxaban), please tell your doctor or the nurse as you may need to stop them temporarily before your
surgery. Also tell your doctor or nurse if you have diabetes as you may need to alter the dose of your diabetes medicines, as you will need to fast before the procedure. Further information on stopping any medicines will be given to you when you come for pre-assessment. Please ask us if you have any questions.
Please let us know if you are taking any regular medicines (including anything you buy yourself over the counter or any herbal or homeopathic medicines) and if you have any allergies to any medicines.
Diet
It is helpful if you can follow a healthy diet, including fresh fruit and vegetables in your daily consumption.
It is important you maintain a good fluid intake, aiming to drink between 2-3 liters during a 24 hour period to prevent a urinary tract infection (UTI) this can be water, sugar-free squash, juices, but limit tea and coffee.
Exercise
In the time between seeing your surgeon in the clinic and having your surgery, it is helpful to try to maintain being as active as possible. This can be as simple as walking to the shops or using the stairs rather than the lift.
If you can do 20 minutes, four times a week, of fast walking, this will help with your fitness and recovery from surgery.
Giving my consent (permission)
We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and you understand what it involves.
What happens on the day of my surgery?
- Fasting instructions: Please do not eat or drink anything (except non-fizzy water) for six hours before your appointment. This means that you cannot suck on sweets or chew gum. You are allowed to drink water up to two hours before your appointment. If you continue to eat or drink after this, your surgery will be canceled.
- Hospital admission: After admission and during surgery, you will be having the surgery under general anesthetic, which means that you will be asleep the whole of the operation and will not feel any pain. The anesthetist will put a cannula (a thin tube into a blood vessel) through which the medications are given to put you to sleep. The anesthetist will see you in your room before surgery to check all is in order for your procedure.
You will be seen by the nurse and a checklist will be completed. You will be asked to put on a hospital gown and special stockings to reduce the risk of developing blood clots in your legs.
There may be a wait before you go to the theatre, depending on where you are on the list.
You will walk to the theatre accompanied by a nurse. Once in the anesthetic room, you will be asked to lie on the trolley and you will be attached to a heart monitor and a cuff placed on your arm to monitor your blood pressure.
Your overnight bag will be labeled with your name, stored securely and taken to the ward for you.
You may be given a daily blood-thinning (anticoagulant) injection and asked to wear anti-thrombosis stockings. This reduces the risk of you developing a blood clot in the leg or lung. These injections may need to be given for 28 days in total and will therefore need to be continued after you have left the hospital. You or a family member/friend will be taught how to give these injections before you leave the ward.
What happens after the surgery?
You will wake up in the recovery room with a catheter in your bladder, a wound drain from your tummy, and four to five small wounds from where the incisions have been made. The incisions may be closed with either suture (stitches) or surgical clips. These are normally removed 10 days after your operation.
You will be monitored in the recovery room and once you are stable you will be transferred back to the ward. We do ask that you move your feet and wiggle your toes to help promote circulation in your legs while you are immobile and bed-bound.
Your catheter will remain in for about 24 hours and the drain will come out after about 48 hours.
The average length of stay in the hospital for this procedure is two to three days. You will be able to leave the hospital when:
• you have passed wind
• you are able to move around safely
• you are able to pass urine
• your pain is well controlled with the painkillers we are giving you.
What can I expect after I go home?
You should remember that although you may feel well and do not have a large scar, you still have had major surgery. You will need a period of time to recover fully before returning to normal activities. You should be active within your home and build up to returning to your usual tasks.
You may have some pain associated with the surgery and it is also common to feel lethargic after major surgery. You may need to rest or sleep more than usual in the first two weeks after the operation.
Will I have a follow-up appointment?
Yes. You will have a follow-up appointment with Dr. Gandhi, 1 week after your surgery, to find out the results from your surgery in room no 107, cancer building no. 8, Ruby Hall Clinic, Road, Pune.
Your follow-up protocol after this will depend on your cancer type. This will be explained to you by Dr. Gandhi when you attend your first follow-up appointment.
Some commonly asked questions
1.Does the robot do the surgery?
No, the surgeon does the operation. The robot allows the surgeon to operate in small spaces in the body. It essentially makes the surgeon’s hands two seven-millimeter instruments. The robot is controlled by the surgeon and does not work on its own.
2.How much pain will I be in after the surgery?
Since the surgery is done through small incisions, most patients experience much less pain than with open surgery, and will therefore require less painkillers. You will be given regular painkillers by mouth or injection for the first few days. After one week, most patients will not experience any pain.
3. When can I exercise?
We encourage light walking right after the procedure and brisk walking after two weeks. Four weeks after the surgery you can resume jogging, aerobic exercise and heavy lifting.
4. Can I shower or bath?
Yes, the stitches in your tummy are either dissolvable or waterproof clip. It is important that you rinse the soap thoroughly from your body as this may irritate the wounds, and that you pat yourself completely dry.
5. When can I drive?
When you are comfortable to do so and when you are able to perform an emergency stop. Please also check with you insurance company before returning to drive.
6. When can I have sex again?
This will depend on when both you and your partner feel comfortable but it is safe after one week.
7. When can I return to work?
Please allow a couple of weeks’ recuperation before returning to work. If your work involves lifting, please speak to your doctor before leaving hospital.
If you have any further questions, please do not hesitate to speak to the nursing or medical staff.
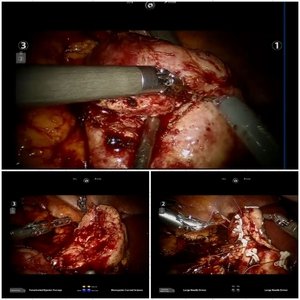
Gallery